Information is useful and applicable when recorded. And if we talk about client progress in mental health treatment, recording becomes obligatory.
Why so?
Clinical notes really help to structure information about the client and his case, to notice some repetitive details, to put together a puzzle, let's say. Moreover, you can track efficiency and progress (and regression too).
A mental health progress note is a convenient tool for keeping track of patients' mental health. Clinicians use note-taking to track patient progress, to state patients’ mental status and to provide patients with an effective and affordable treatment plan.
A plan section in a medical professional note is another reason. It’s sometimes necessary to make adjustments to a treatment plan during or after a session. And when you attend a supervision-intervention, or transfer clients to another therapist, such records are very much in demand.
In contrast to different note-taking styles, SOAP progress notes will help you share patient assessment and plan with other health professionals in an organised manner.
Learn how to simplify your practice workflow and free up more time for patients with Medesk.
Open the detailed description >>After all, it's not for nothing that doctors always keep medical records? It probably makes sense.
In this article we’ve got you covered on:
- What is a SOAP format
- Tips for writing mental health SOAP notes
- Examples, and more.
What is a SOAP format?
The SOAP framework combines four core elements, in other words four specific letters in the acronym: Subjective, Objective, Assessment, and Plan.
These four elements, or stages, represent a sufficient structure of recording information for mental healthcare providers, capturing data about a client, his family and background, chief complaints, and certain aspects of the session.
The subjective part includes the client's condition, while the objective part provides some quantifiable data (tests, questionnaires, etc.). Assessment refers to the analysis of therapy sessions. And finally, the Planning stage contains treatment goals to be achieved.
Mental health SOAP notes are mainly used to record psychotherapy observations, but that’s not the only benefit. This kind of patient note helps healthcare professionals to pass through all the workflow stages during patients’ treatment, such as:
- Scheduling and rescheduling (including follow-ups)
- Check-in and examination
- Billing
Now we will consider all four stages and find out how to make the very most out of each one. Let’s get started.
Medesk helps automate scheduling and record-keeping, allowing you to recreate an individual approach to each patient, providing them with maximum attention.
Learn more >>Subjective
The subjective section includes the client’s condition. Here a clinician puts down information concerning the client’s biggest complaint, and also adds other relevant information from the client. It’s better to use direct quotes at this stage to be fully unbiased, because your priority now should be to seize a full picture of the symptoms that bother your client. Also, if it’s a follow-up visit, you may write down some progress from the previous session.
For instance, you may include such quotes as:
Mary says, “I had a terrible headache.”
Steven complains, “My nightmares never end.”
After the direct speech, it’s important to point out the elements of your further discussions about the given symptoms.
We think the type of information to avoid in the Subjective part needs to be noted.
Always try to avoid making assumptions, if they are not supported by the facts. In other words, in this point of note-taking, only information obtained from the client, his relatives, teachers, and friends can be attached, allowing you to get a sense of his mood, desires, and motivation. Don’t make it up.
Objective
The objective section, as you can see by its name, provides some quantifiable data (tests, questionnaires, etc.). Objective data contains the results of the physical exam, including the differential diagnosis, physical symptoms, mood, affect, body language and behavior of the patient.

Here, if compared with the objective part, you can use your personal observations about the client’s behavior, for example:
- Is he nervous/talkative/twitching?
- What does his body language tell you? Is he cooperative or withdrawn?
- Is he able to participate in the session
- When and how do his responses occur?
Here you can also add the results of psychological tests, questionnaires and previous medical records if they are applicable.
For instance:
“Steven takes several seconds to answer my questions. The eye contact is very poor, he leans back, arms crossed.”
Again, try to avoid value judgments, labels and words with negative connotations, such as stubborn, rude, or childish. Negative attitudes and judgments quickly take root in the mind of a person with psychological problems. You are here to help, not to judge.
Assessment
The assessment section refers to the analysis of therapy sessions. Its main goal is to combine the S and O sections, and interpret the professional information received during the session.
At this stage a healthcare professional implements the Diagnostic and Statistical Manual of mental disorders (DSM), meaning that he identifies its criteria, vital signs, themes and individual patterns of a patient’s mental status.
Put another way, here you can use specific psychiatric and psychological terms and abbreviations, such as abundance of guilt, anxiety, moderate depression, anxious distress, melancholy, ECT, TMS, VNS, persistent depressive disorder and other. You can also share information about whether a client meets the criteria for generalized anxiety disorder, known as GAD, as a common mental health problem.
Furthermore, you should avoid repeating your previous statements in the S. O. sections. Progress and regression are reported in the assessment section.
Planning
In the planning stage, there are treatment goals that need to be met. This is the plan for a client, so he can see how to reach the long term goals you’ve set together.
Discover more about the essential features of Medesk and claim your free access today!
Explore now >>Here your task is to focus on the following:
- Steps for the follow-up appointments
- The symptoms to pay attention to next time
- Treatment plan assessment (or reassessment).
For example, it can be used to add nutrition consultation, to run additional analyses, or even to change a lifestyle plan.
Remember to set realistic and measurable goals, so that a client can achieve them before the next session. Reaching small goals within a larger plan has a positive effect on the entire treatment.
Needless to say, SOAP note templates facilitate next sessions, combining objective and subjective information for better therapy notes.
In addition, they impact the patient journey from the moment they develop symptoms and schedule a doctor's appointment to the moment they complete medical treatment. If you know the clinical reasoning behind why, when and what you do to cure someone, then it is always an advantage.
8 tips for writing mental health SOAP notes
A mental health professional has a lot of responsibilities during and after the session. Sometimes making up a workable soap note format can be a challenge. To make things easier for you, we’ve summarised the top 8 tips to focus on when writing your notes:
- Keep in mind avoiding moral and value judgments
- When you use direct speech, make sure that you cite the exact words
- Avoid any uncertainty, for example, such words as “may“, “seem”, “appear“
- Always write legibly, without incomprehensible abbreviations
- Use special language and professional jargon
- Mind your grammar and spelling, don’t forget to proofread
- If you still have any doubt in writing the SOAP notes then use AI tools such as a free sentence improver. This tool helps improve the overall quality of your notes while saving you time.
- Imagine that you are about to defend the content of your note. Write it accordingly.
And here is one extra tip for you.
If you are working with patients remotely, via telehealth or telemedicine, SOAP note examples are also required. As a result, switching from paper to EHR ensures proper security of your notes that you do not want to lose.
You should include:
- Date and time of the appointment
- Time of the follow-up visit
- Mental status
- Type of connection (telephone, video conference, chat)
- Location of the medical provider (home/office)
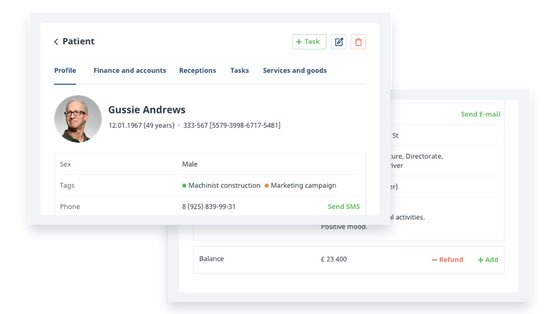
Digital SOAP notes can be filled directly into the patient's medical card during or after the consultation, thanks to the embedded mental health progress note templates. This option encourages efficiency, coherence, and care consistency.
