The diagnosis of cancer is made annually to more than 370 000 people in the UK. Recent oncological statistics show an increase in cancer patients. The struggle for the patient's life and the quality of it begins with research for the formulation of an oncological diagnosis - oncology history-taking.
This process involves gathering detailed information from patients about their medical background, presenting symptoms, lifestyle, and family history. By recording this information, healthcare professionals can gain invaluable insights into the patient's unique health profile, enabling personalized and effective cancer care.
Learn how to simplify your practice workflow and free up more time for patients with Medesk.
Open the detailed description >>Then, if there are indications, the patient is referred to additional stages of oncology diagnostics: blood tests, urine, feces, ultrasound, tomographic, X-ray, endoscopic studies, etc.
In this article, we will discuss the stages of history-taking and physical examination in oncology in more detail, exploring its significance, essential components, and communication strategies.
The Significance of Oncology History-Taking
Scrupulous oncology history-taking is more than just a routine procedure. It is the gateway to a comprehensive understanding of the patient's condition. By collecting pertinent details about the patient's medical history, symptoms, and risk factors, clinicians can make informed decisions about the most appropriate diagnostic tests, treatment options, and follow-up plans. This personalized approach can significantly improve patient outcomes and enhance their overall quality of life.
How to Prepare?
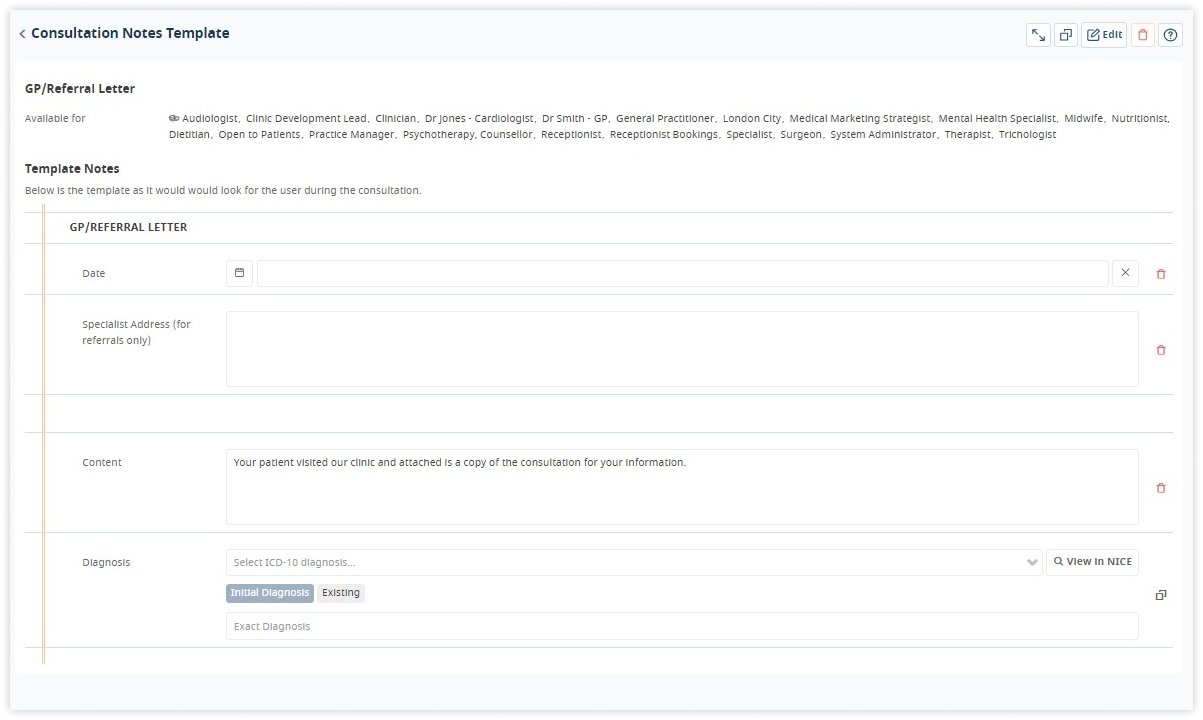
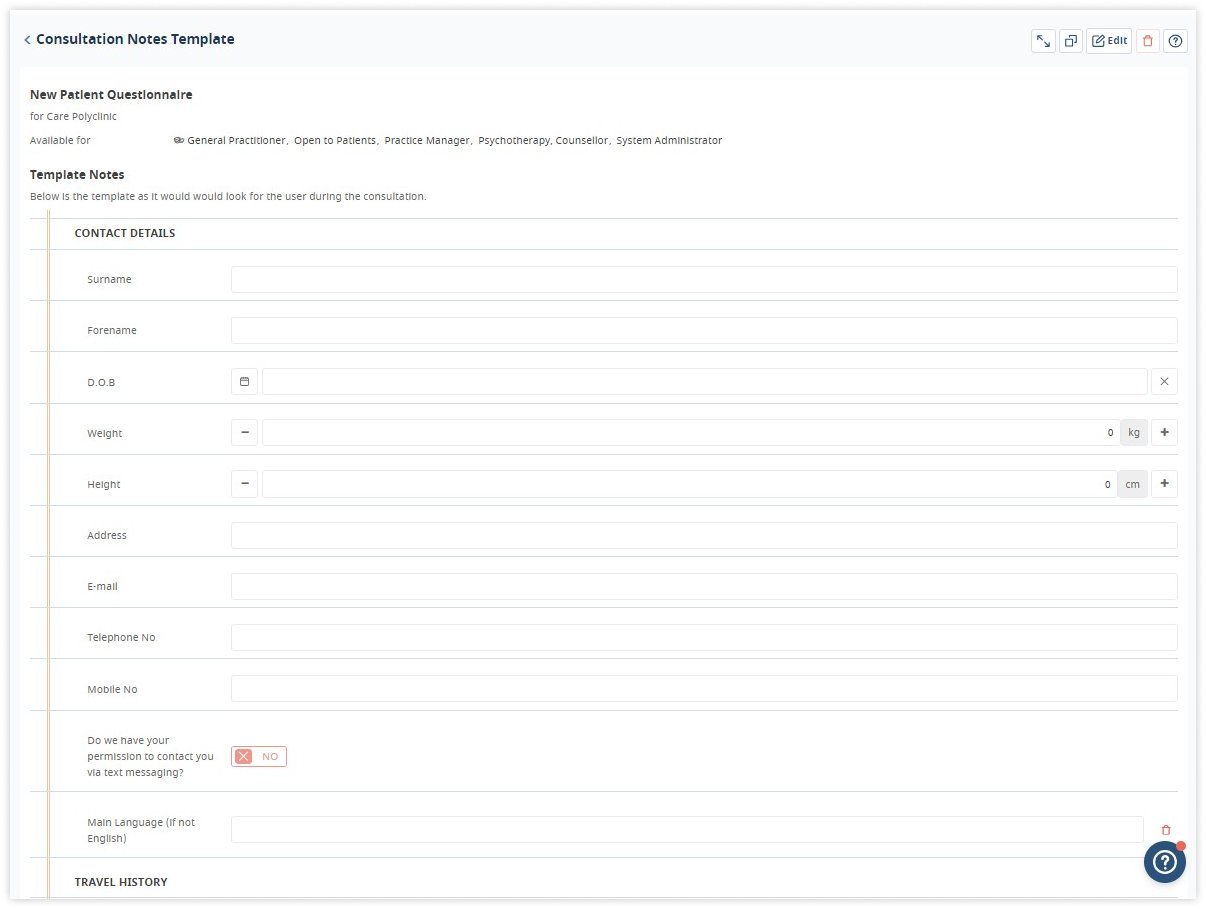
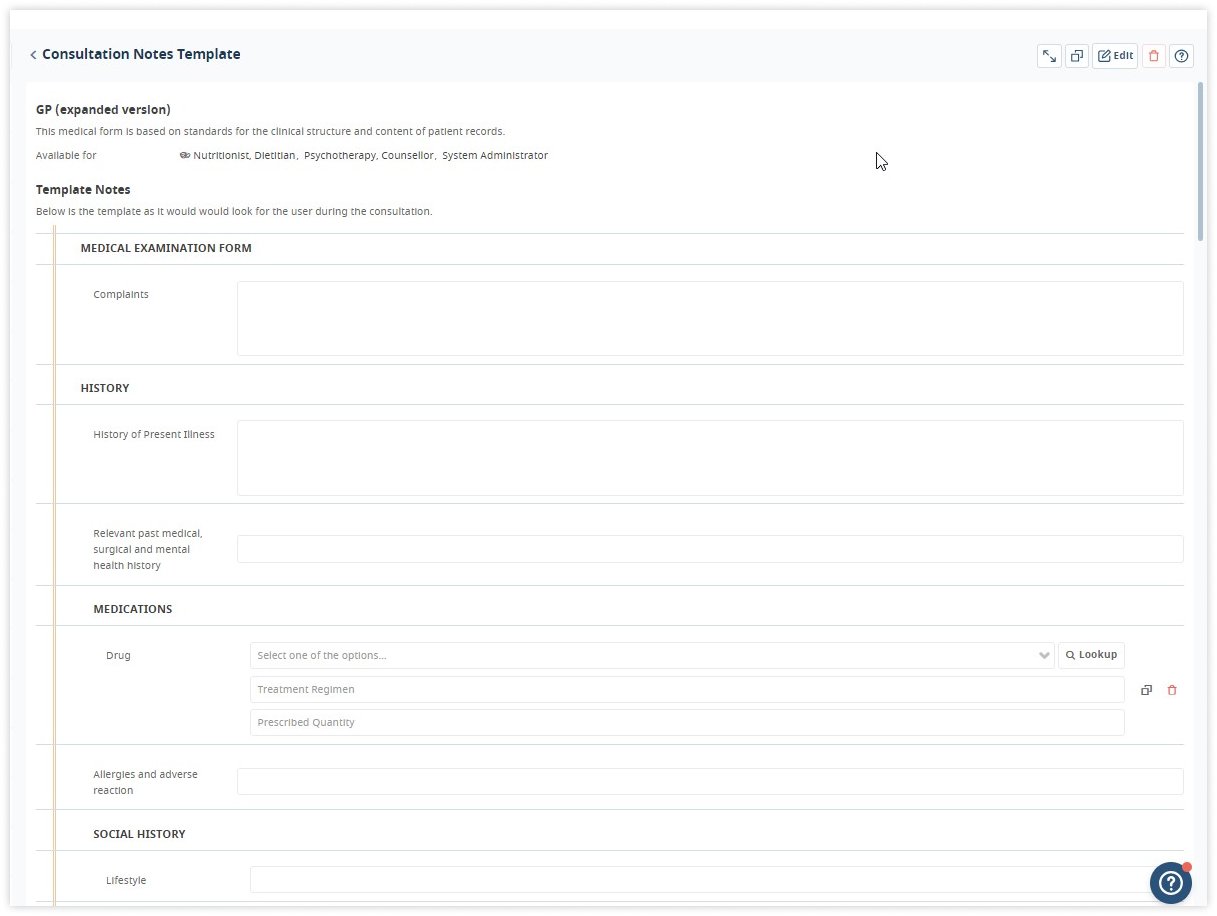
Creating a favorable environment is essential for successful oncology history-taking. Practitioners must ensure that patients feel comfortable and supported during the process. We recommend equipping yourself with the necessary tools, such as a detailed questionnaire and access to electronic health records.
Medesk helps automate scheduling and record-keeping, allowing you to recreate an individual approach to each patient, providing them with maximum attention.
Learn more >>Establishing rapport with the patient and their family members fosters trust and open communication, allowing for a more accurate and comprehensive history.
Essential Components of History-Taking
Examination of cancer patients should be strictly systematic and based on consistency. Analyzing complaints and collecting anamnesis are the most important factors, and no detail should be overlooked.
Patient's demographics and chief complaint
The doctor and patient meet to discuss complaints. The doctor should listen carefully to the patient, not interrupting him, but only helping with leading questions. The thoroughness of the patient's survey is especially important for the diagnosis of a malignancy with internal localization.
It must be remembered that in the early stages of malignant tumor development, the patient may not make certain complaints. This is except for persons with long-term pre-tumor diseases of a particular organ.
Present illness history
A clinician gathers a detailed account of the patient's current symptoms, including associated factors, aggravating or alleviating factors, and any changes over time.
Paying attention to pain, it is necessary not only to clarify its localization and irradiation, but also to note the change in character, seasonality and duration. At the same time, it should be remembered that pain is not characteristic of early cancer and is more characteristic of a far-reaching process.
The doctor should be alarmed by fatigue, drowsiness, loss of interest in the environment, decreased performance, etc., which appear against the background of complete well-being (the so-called small symptoms of malignant lesions).
Past medical history
Examining the patient's medical past helps identify pre-existing conditions that may impact cancer treatment decisions. Additionally, understanding the family's history of cancer and other relevant diseases can highlight potential genetic factors.
Natural anamnesis is what the patient tells himself about his illness:
- the onset and dynamics of the development of the disease
- in the opinion of the patient, the causes of its occurrence
- the presence of pre-tumor diseases, etc.
The forgotten anamnesis is the additional information that the patient reports, answering clarifying questions about the present disease (date of treatment, examination and treatment), transferred diseases that can serve as a background for the development of a tumor, profession, hereditary predisposition to cancer.
The presence of transferred or existing diseases (blood, kidneys, cardiovascular system and other vital organs), which may limit the possibility of follow-up and influence the choice of treatment methods, must be considered.
In the presence of a tumor pathology associated with gynaecology (breast cancer, uterine cancer etc.), it is necessary to clarify the state of menstrual function:
- the time of the onset of menstruation
- duration, periodicity and cyclicity of menstruation
- the age at which menopause began.
Medication and allergies
Knowledge of the patient's current medications, side effects and allergies is critical to safe and effective cancer treatment.
Lifestyle, social history and environmental factors
Evaluating lifestyle choices, such as smoking, alcohol consumption, diet, and exercise, along with occupational and environmental exposures, provides insights into potential risk factors.
When living in a territory contaminated with radionuclides, it is necessary to specify the locality, the period of residence, and the time of relocation.
This section of the medical history should reflect:
- working and living conditions that could contribute to the appearance of a tumor (occupational hazards, regularity and peculiarities of nutrition, lifestyle)
- bad habits (smoking, duration of smoking, number of cigarettes per day, alcohol and narcotic substances)
- heredity (the presence of malignant neoplasms in blood relatives).
The presence of allergic reactions, blood transfusions and blood substitutes with tolerability indication is noted.
Review of systems
Conducting a systematic evaluation of other body systems helps detect secondary symptoms related to primary cancer or its treatment.
This section includes a description of the general condition of the patient, as well as the results of a physical examination (palpation, percussion, auscultation) of organs and systems. If the patient does not have a severe concomitant pathology, systems and organs are described briefly.
There is only part of the information provided.
- The patient's general condition: satisfactory, moderately severe, severe.
- Patient position: active, passive, forced.
- Physique: normosthenic, asthenic, hypersthenic, height, weight.
- Body temperature.
- Skin and mucous membranes: coloration (normal, pale, jaundice, earthy, cyanotic, bronze), pigmentation, depigmentation, scars, combs, hemorrhages, rashes, elasticity, moisture, turgor.
- Peripheral lymph nodes.
- Muscles: development degree (good, moderate, weak).
- Joints: change of configuration, soreness and crunch during movements, volume of active and passive movements.
- Bones: deformity, soreness during palpation, limited mobility.
- Neurological status: consciousness (clear, confused); mood (calm, depressed, anxious, euphoria); reaction of pupils to light.
- Thyroid gland: neck shape, visible deformities, symmetry; displacement of the trachea and larynx; tumor localization (right or left lobe, isthmus, pyramidal lobe, total lesion), contours of the tumor (clear, fuzzy); fusion with the skin, with the underlying tissues, ulceration.
- Mammary glands.
Preliminary diagnosis
A preliminary diagnosis is formulated on the basis of complaints, anamnesis, outpatient examination results, and objective research data. There is a description of the histological type of tumor (cancer, sarcoma, melanoma, malignant lymphoma, etc.), location (organ and department), and stage.
Red Flags and Alarm Symptoms
Healthcare providers must be vigilant in identifying red flags or alarm symptoms that indicate immediate attention. Prompt referrals and further investigations are crucial to timely cancer diagnosis and treatment.
Here are some common red flags in oncology history taking:
- Unexplained weight loss
- Persistent pain
- Unexplained fatigue
- Night sweats
- Changes in bowel or bladder habits (e.g., diarrhea, constipation, blood in stools)
- Unresolved cough or hoarseness
- Abnormal lumps or masses
- Unexplained anemia
- Personal or family history of cancer
- Neurological symptoms
- Dysphagia
- Abnormal bleeding
- Suspected paraneoplastic syndromes: endocrine abnormalities.
Adapting History Taking for Different Patient Populations
Understanding the nuances of history taking for diverse patient populations, such as pediatric and geriatric patients, as well as being sensitive to cultural differences, ensures a patient-centric approach to cancer care.
Discover more about the essential features of Medesk and claim your free access today!
Explore now >>Moreover, accurate documentation of history-taking details is imperative for maintaining a complete medical record and facilitating collaboration among healthcare professionals involved in the patient's care.
Practice management software with its built-in templates and consultation notes saves you time during an appointment. There is no need to be distracted by filling out the medical history manually. Do what is really critical - keep an eye on your patients.
Imagine all the advantages of practice management software with an electronic health records module. Don’t hurry, take your time.
And when you are ready, let’s look at the lung cancer history-taking example.
Oncology History-Taking Example: Lung Cancer Patient
This example illustrates a hypothetical oncology history-taking session with a patient diagnosed with lung cancer.
Patient information
Name: John Smith
Age: 58
Contact: john.smith@email.com | (555) 123-4567
Chief complaint
John has persistent cough, chest pain, and shortness of breath for six months. He reports recent weight loss and fatigue.
Present illness
John describes a progressive cough with occasional blood-streaked sputum. Chest pain worsens during coughing, deep breathing, and movement. Shortness of breath has limited his daily activities.
Medical history
John's medical history includes hypertension, but no cancer diagnosis. He had an appendectomy in his 30s.
Family medical history
John mentions no history of lung cancer in his family, but his father passed away due to a heart attack.
Lifestyle and risk factors
John used to smoke two packs of cigarettes daily for 30 years before quitting five years ago. He has a sedentary lifestyle and admits to occasional alcohol consumption.
Medication and allergies
Current medications: Amlodipine for hypertension.
Allergies: None reported.
Social and emotional aspects
John lives with his wife and supportive family. However, he expresses anxiety and fear about the cancer diagnosis.
Review of systems
- Respiratory: Cough, sputum production, dyspnea.
- Gastrointestinal: No specific issues reported.
- Cardiovascular: No palpitations or chest discomfort other than lung-related pain.
- Neurological: No significant complaints.
- Musculoskeletal: Some discomfort due to chest pain.
Physical examination
- General: John appears fatigued but alert.
- Respiratory: Decreased breath sounds on the right side. Dullness on percussion over the right lung base.
- Cardiovascular: Regular rhythm, no murmurs.
- Other systems: Non-contributory findings.
Investigations and imaging
- Chest X-ray: Right lung mass and pleural effusion.
- CT scan: Further characterization of the lung tumor and its extent.
- Biopsy: Pending for definitive diagnosis.
This example demonstrates how conducting an oncology history-taking with a lung cancer patient like John is crucial for understanding the disease's clinical presentation, risk factors, and potential treatment options. Further investigations, such as imaging and biopsy, will confirm the diagnosis.
This will enable the oncology team to formulate an appropriate and personalized treatment plan for John's lung cancer. Emotional and psychological support provided during this process is essential in helping patients cope with their diagnosis and treatment journey.
Final Thoughts
A well-documented oncology history provides valuable insights for oncologists to formulate accurate diagnoses and personalized treatment plans. Empathy, compassion, and active listening are essential during this process, as patients may share sensitive information and emotions related to their health journey.


