Electronic health records system implementation can be a difficult process, particularly because it affects your medical practice’s workflow.
As such, you have to make sure your EHR implementation process goes smoothly—otherwise, it may disturb your clinic’s performance and result in hidden costs.
So, if you’re looking for a step-by-step guide that will help you ensure a successful EHR implementation cost breakdown, we’ve got you covered!
In this guide, we will go through everything there is to know about EHR implementation, including:
- 4 Phases of EHR Implementation
- 10-Step Checklist for EHR Implementation
- Best Practices for Successful EHR Implementation
- EHR Implementation Challenges
- Cost of EHR implementation
After reading this, you will be able to fully understand the intricacies of implementing electronic records in your clinic, and you will also learn a couple of lifehacks on how to get your clinic up and running with the new software. Enjoy!
Learn how to simplify your practice workflow and free up more time for patients with Medesk.
Open the detailed description >>4 Phases of EHR Implementation
Before we cover anything else, let’s start with the 4 phases of successful EHR implementation:
1. Planning and selections. Before starting the EHR implementation process, you should create an EHR implementation plan. This way, you can ensure that the EHR implementation process goes smoothly. At this stage, you should also research various EHR systems and choose the one that best fits your medical practice’s needs.
2. Adaptation and implementation. It’s important that you prepare your staff to transition to an EHR system. As such, make sure to involve your staff in the change management process by providing them with EHR training. It’s also useful to educate both your staff and your patients about the benefits of EHR.
3. Optimization and workflow redesign. Use the feedback from your staff and patients to effectively optimize your EHR system and redesign the workflow for maximum efficiency. Make sure that you optimize your EHR system regularly, as your practice’s needs and requirements may change over time.
4. Data migration and training. If your medical practice is expanding, you may find that your EHR system no longer suits your needs. As such, you might want to migrate your medical data to another EHR system. Providing your staff with the necessary training can help your practice to provide data security and increase patient satisfaction.
10-Step Checklist for EHR Implementation
EHR implementation is a complicated process, so it’s crucial to break it down into easily manageable steps.
Here’s our 10-step EHR implementation checklist that can help guarantee a smooth and successful EHR adoption process:
#1. Create Your EHR Implementation Plan
A detailed EHR system implementation plan is the cornerstone of a successful EHR rollout. For this reason, it’s important that your plan outlines all of the tasks that need to be completed throughout the entire process.
Here are some of the key tasks that you should include in your EHR implementation plan:
- Form an EHR implementation team
- Define the cost of implementing electronic information system
- Select the best EHR software for your healthcare organization
- Transfer your medical practice and patient data to the EHR system
- Provide your staff with EHR training and define training costs
- Test your cloud-based or on-premise system
- Define your go-live approach
- Collect feedback on the data transfer and EHR implementation.
Medesk helps automate scheduling and record-keeping, allowing you to recreate an individual approach to each patient, providing them with maximum attention.
Learn more >>#2. Form Your EHR Implementation Team
Once you have outlined your EHR implementation plan, you need to form a team that will execute the tasks you’ve planned. This way, you can be sure that your EHR integration goes in accordance with your schedule and budget.
Depending on your medical practice’s needs and budget, you can either assign tasks to your current clinical staff members or hire new employees to carry out the tasks.
Here are some of the key roles you need to form an effective EHR implementation team:
- The project manager is responsible for communicating with the EHR vendor and staff, as well as tracking the implementation progress.
- EHR superuser, who is the information technology expert responsible for creating templates, developing workflows, training staff, and creating standards for dealing with any disruptions related to using the EHR software.
- Lead clinician, who represents all physicians in a practice and is responsible for planning and implementing physician training.
- Lead nurse, who represents all nurses and is responsible for planning and implementing nurse training.
- Billing advocate, who represents the billing department and is responsible for planning and implementing billing department training.
- Application developer, who is responsible for customizing the EHR system to fit your practice’s needs.
- Application analyst, who is responsible for data migration and data backups.
- Software tester, who is responsible for testing your EHR system and its usability.
If your budget allows, you might also want to consider hiring an EHR implementation specialist. This person helps you with many of the tasks outlined above, including data migration, staff training, EHR testing, and more.
#3. Schedule Your EHR Implementation
By now, you should be ready to schedule your EHR implementation based on these 3 factors:
- Project scope
- Team (size and efficiency)
- Budget and software cost.
Rollout time varies for each practice, but taking these three factors into consideration can help you effectively schedule the implementation timeline.
Nonetheless, EHR implementation is a lengthy process—it typically takes up to 8 months for a medical practice to fully adopt EHR, excluding the time spent planning and decision-making.
#4. Determine Your Requirements For EHR Software
Besides storing and organizing your electronic health records, EHR systems usually offer a variety of other features that can enhance your medical practice.
As such, you want to consider your practice’s specific needs and requirements to choose the best modules for your medical practice.
Some of the features that EHR software offers include:
- Automated appointment scheduling
- Clinical document generation
- Reporting and data analytics
- Telemedicine
Look for software that will provide as many features as possible at an affordable price. Just because you don't need a telemedicine and payroll module yet, doesn't mean you won't need it a year from now. Why not choose a system that is designed for the potential growth of your practice?
_With Medesk, you get 20+ modules that you can turn on and off as you see fit at no additional cost. Sign up today and get 15 days free to use all the features of the platform. No credit cards, calls, or other time-consuming activities required._

#5. Reach Out to Vendors
Once you have a clear list of requirements, your project manager or EHR implementation specialist can research potential vendors and start reaching out to them.
To do this, they will need to submit two requests to prospective vendors:
Once these requests are returned, you can evaluate the vendors based on your requirement list and make a list of the top 3 EHR vendors for you.
#6. Select The Best Vendor
To select the best vendor for your medical practice, you should require a demonstration from the vendors on your shortlist.
This demonstration typically includes a presentation of the EHR system and its simulation. It also provides you and your team a chance to get answers to your questions. But the better option is to start a free trial and see everything for yourself. Additionally, you can leverage an AI RFP to streamline vendor proposals, quickly compare features, and make a more data-driven decision on which EHR system fits your practice best.
By everything, we also mean the speed of the support team's response. All software has failures, so you should evaluate the training centre and the specialists' answers before choosing a solution.

After seeing and comparing the demonstrations, you should be ready to select the best vendor for enhanced patient care and negotiate the contract.
#7. Evaluate Your Hardware Needs
Once you have selected the EMR software, the next step is to consider your hardware needs.
These will largely depend on your requirements, budget, and office space.
For example, some medical practices have a printer in each room and provide all staff members with individual laptops to increase efficiency and save time; however, this may not be the best option if you’re on a tight budget or operate a small practice.
#8. Transfer Your Medical Data
The next EHR implementation step is to transfer your medical data into your EHR system.
Here’s what you need to do:
- Convert paper records to electronic records
- Cleanse and verify data
- Set up a patient information database
- Transfer data to your EHR system
- Test and verify legacy data and new data inputs
To help you with the process, you can also make a checklist of all the data you want to transfer to your EHR system.
#9. Train Your Employees
Medical staff training is an integral part of any EHR implementation plan that helps your practice to successfully transition from paper records to an EHR system.
Here are some tips that can help you to prepare an effective training program:
- Take your time. EHR medical staff training can be quite challenging, especially for employees that aren’t tech-savvy. So, start with the basic elements of using an EHR system in your practice. Once all staff members are comfortable with the basics, you can introduce additional training to improve skills, learn all the time-saving shortcuts, etc.
- Provide role-based training. Role-based training ensures that each staff member knows exactly how to use the EHR system for their specific job. This way, role-based EHR training helps your employees to work more efficiently and independently.
- Let employees train their colleagues. Train the most tech-savvy employees in each role to effectively use the EHR system and teach their colleagues. This can increase your training’s efficiency as, for example, your lead nurse likely knows the best approach to teaching other nurses compared to your accountant.
- Listen to feedback. Make sure to collect feedback after each EHR training session to improve your training. Moreover, planning training sessions that match your employees’ needs may also be of help.
- Plan ongoing training. As time progresses, you’ll need ongoing training to introduce your staff to new features, functions, and tools. Not to mention, ongoing training allows colleagues to share their time-saving tricks, shortcuts, and new ways of using and making the most out of your EHR system.
Medesk helps automate scheduling and record-keeping, allowing you to recreate an individual approach to each patient, providing them with maximum attention.
Learn more >>#10. Prepare For Your Go-Live Day
Once your staff is comfortable and skilled in using the new EHR system, it’s time to plan how to launch it.
There are two main go-live approaches:
- Going all in. With this approach, you introduce the EHR system with all its features to your practice at once. While this approach can help you save time, it can also be challenging if your practice isn’t prepared to tackle the issues or novelties that may arise during the launch.
- Going slow and steady. Using this approach, you introduce EHR system features one by one. For example, you can start with introducing automated appointment scheduling, then introduce medical billing features, etc. This way, your staff and patients alike can ease into using the EHR system.
On the actual go-live day, it’s generally advised to lower your patient volume and inform your patients in advance that your practice is transitioning to an EHR system.
This way, you can make sure that your EHR implementation goes as smoothly and stress-free as possible.
Best Practices for Successful EHR Implementation
Here are some of the best practices that can help you ensure a successful EHR implementation:
- Ensure HIPAA compliance. To avoid violating HIPAA, make sure to follow the security measures and see if the software is HIPAA compliant before you adopt it. To do this, you may want to organize a HIPAA risk assessment.
- Prepare for the unexpected. It’s very likely to run into some unexpected issues, such as a power outage or system malfunctions, during your EHR implementation process. As such, it’s important that you brainstorm potential issues and plan how to handle them in advance.
- Collect feedback. To make the most out of your EHR system, make sure to regularly collect feedback from your employees. This way, you can improve and customize your system for your medical practice.
- Measure EHR implementation metrics. Tracking EHR implementation metrics, including end-user satisfaction, calculating return on investment (ROI), and monitoring EHR staff training rates, can help you to evaluate your EHR implementation success and improve the process.
EHR Implementation Challenges
Without the necessary preparation, you may run into some challenges during your EHR implementation process, including:
- Workflow breakup. The goal of using an EHR system is to optimize your practice’s workflow. An EHR solution that isn’t customized for your medical practice, however, may disturb your workflow. As such, make sure to ask the vendor to demonstrate how your practice should implement and customize the EHR system.
- Insufficient training. Your EHR system is only useful if your employees know how to effectively use it. However, staff training takes time and effort, and may be expensive, so make sure to plan your staff training needs in advance.
- Costs. Maintenance costs can be expensive. For this reason, one of the first EHR implementation steps is to carefully plan your budget to make sure that your practice can afford it.
Discover more about the essential features of Medesk and claim your free access today!
Explore now >>EHR Implementation Cost Breakdown
Implementing an electronic medical records system expenses are categorised into initial setup costs, ongoing operational costs, and indirect costs.
Initial setup costs (upfront costs)
They include:
- Software licensing fees for purchasing or subscribing to the EHR software.
- Customisation costs tailor the system to the practice's specific needs.
- Hardware costs encompass purchasing servers, storage solutions, workstations, computers, tablets, and necessary network infrastructure like routers and switches.
- Implementation services cover consulting fees for planning and implementing the EHR system, along with costs associated with installation and configuration.
- Training and support costs are significant as well.
- Data migration costs.
Ongoing operational costs
Ongoing operational costs include:
- Subscription fees for cloud-based EHR systems cover software updates and technical support.
- Ongoing maintenance and support costs involve regular software updates and continuous technical support.
- Hardware maintenance includes periodic upgrades and replacements of hardware components.
The average costs for ongoing operations in a small to medium-sized practice in the U.S. typically range from $4000 to $24,400 per user per year. The larger the healthcare provider, the higher the cost.
Indirect costs
Indirect costs comprise productivity losses due to the learning curve associated with the new system and the potential need to hire temporary staff during the transition period.
Compliance and security costs involve ensuring the EHR system complies with healthcare regulations such as HIPAA and GDPR and implementing measures to protect patient data.
The first-year total cost of ownership ranges from $16,400 to $68,400 per provider.
Try Medesk for Free and Cut Your Implementation Costs
If you’re looking for professional EHR software that will enhance your medical practice, try Medesk!
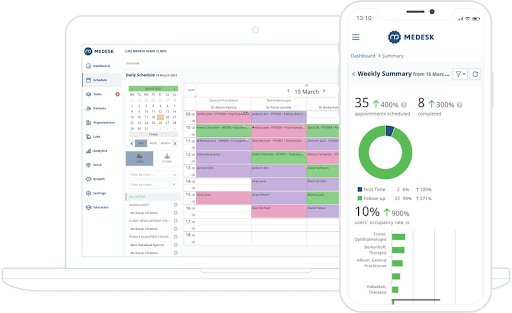
Medesk is an integrated practice management software that comes with a variety of useful features to help you manage all aspects of running your medical practice, including:
- EHR: store, organize and manage your patient medical records and health information securely in your EHR system.
- Online booking: let your patients easily book appointments online with the click of a button.
- Medical billing: conveniently manage all of your payment processes directly in the Medesk PMS.
- Stock reporting: use this tool to manage your inventory, generate stock reports, and calculate your practice’s profitability.
- Scheduling tool: send automated appointment reminders to your patients, reduce no-shows, and easily manage your schedule.
Join thousands of our satisfied customers who are switching to Medesk from other practice management software.

Sign up for free and get 15 days of access to the full functionality of the platform. Our support team will show you how one platform can improve the quality of care and cut implementation costs in half! Click the link below ↓


